
Mitch Patrick MD 1, David Kuehn MD 2, Rami El Abiad MD 3, Frederick Johlin 3, Daniel Katz MD 4
1Department of Surgery, University of Iowa Hospitals and Clinics, Iowa City, IA 52242, USA.
2Department of Radiology, University of Iowa Hospitals and Clinics, Iowa City, IA 52242, USA.
3Department of Internal Medicine, Gastroenterology-Hepatology Division, University of Iowa Hospitals and Clinics, Iowa City, IA 52242, USA.
4Department of Surgery, Division of Transplant, University of Iowa Hospitals and Clinics, Iowa City, IA 52242, USA.
*Corresponding author: Mitch Patrick, Department of Surgery, University of Iowa Hospitals and Clinics, Iowa City, IA 52242, USA.
Received: December 22, 2023
Accepted: December 26, 2023
Published: December 29, 2023
Citation: Patrick M, Kuehn D, Rami E Abiad, Johlin F, Katz D. (2023) “Resolution Of Efferent Limb Small Bowel Obstruction from Enterolith and Bezoar Using Endoscopy in Patients with Roux-En-Y Reconstructions.”. International Surgery Case Reports, 5(2); DOI: http;//doi.org/07.2023/1.1067.
Copyright: © 2023 Mitch Patrick. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Obstructing enteroliths or bezoars at Roux-en-Y surgical reconstructions are rare complications not always considered in the differential of afferent and efferent limb syndromes. When identified, management has typically been surgical.
Case Presentation: Herein we report 2 cases of small bowel obstruction and another of chronic abdominal pain likely from intermittent obstruction, managed successfully with endoscopic techniques. A discussion of the clinical and radiologic presentation as well as predisposing factors with attention to the existing literature is presented.
Conclusion: We advocate consideration of endoscopic management of Roux obstructions due to enterolith or bezoar given the presence of institutional facilities, equipment, and expertise.
Introduction:
Bezoars are conglomerations of indigestible material that accumulate in the gastrointestinal (GI) tract, most commonly in the stomach. They are an uncommon cause of GI symptoms and bowel obstruction. Bezoars are classified according to the type of ingested material that forms the obstructive concretion, such as vegetable matter (phytobezoar), hair (trichobezoar), or medications (pharmacobezoar) [1]. Underlying altered anatomy such as bariatric surgery or bowel dysmotility problems like gastroparesis can predispose to bezoar formation [2]. Although bezoars may migrate from the stomach into the intestine, primary formation of bezoars in the small intestine is rare and accounts for less than 5% of cases of small bowel obstruction [1].
Afferent limb associated enterolith formation is also known to be an uncommon cause of afferent limb syndrome and cholangitis following hepaticojejunostomy [3]. Bezoar and enterolith formation share gastrointestinal motility and stasis-related risk factors, although enterolith formation may uniquely require the pH lowering conditions created by the diversion of intestinal contents which engender biliary salt precipitation [4]. In addition, bacterial overgrowth has been implicated in enterolith formation due to the bacterial induced deconjugation and precipitation of bile salts [5].
Endoscopic management of gastric bezoars has been described; nevertheless, the exact role of endoscopy in obstructing small intestinal bezoars and enteroliths is not as well defined. This is perhaps a result of several factors including the technical expertise required to perform the procedure, treatment algorithms that advocate operative management for small bowel bezoars, and the likelihood that some bezoars and enteroliths lodge beyond the reach of the endoscope [6].
This report describes three unusual cases of small bowel obstruction caused by bezoar and enterolith at the level of the jejunojejunostomy anastomosis in two patients who underwent prior Roux-en-Y hepaticojejunostomy anastomoses and one that underwent a Roux-en-Y gastric bypass. To our knowledge, there are only 9 prior reports of jejunojejunostomy associated bezoar and enterolith, none of which were managed successfully with endoscopy.
Case Presentation:
Case 1:
Patient number 1 is a 53-year-old female who underwent Roux-en-Y hepaticojejunostomy in March 2012 to repair an extrahepatic bile duct injury that occurred during laparoscopic cholecystectomy. This injury was defined, but not resolved with endoscopic retrograde cholangiography and stenting. In addition to the chronic cholecystitis with choledocholithiasis which formed the indication for the cholecystectomy, the past medical history included colon polypectomy (tubulovillous adenoma), endometrial ablation, tubal ligation, and gastroesophageal reflux disease. She was a nonsmoker and light occasional consumer of alcohol. Two years later, the patient presented with jaundice, abdominal pain, bloating, and mild hyperbilirubinemia and transaminitis (total bilirubin 1.7 mg/dL, aspartate aminotransferase 73 U/L, alanine aminotransferase 132 U/L). The white blood cell count, amylase, and lipase were normal at that time. Following unsuccessful management with percutaneous transhepatic cholangiography and stenting of a stenotic right posterior duct stricture, a right hepatic lobectomy with hepaticojejunostomy revision to the left duct was performed 26 months after the initial surgery. Six months later the patient presented with three weeks of worsening nausea and abdominal pain exacerbated by eating. Her medications included ursodiol, docusate PRN, omeprazole, and sennosides daily. Bilirubin, transaminases, amylase, lipase and white blood cell count were normal. A computed tomography (CT) scan of the abdomen showed heterogenous material at the jejunojejunal anastomosis suspicious for bezoar. The bezoar was retrieved endoscopically using Roth net and braided snare via antegrade double-balloon enteroscopy. The afferent limb was examined to the level of the hepaticojejunostomy and the efferent limb was examined 50 cm distally without evidence of pathology, strictures, or kinks. The anastomosis was widely patent with no evidence of stenosis or ulceration. She has since been managed with a low residue, low-fiber diet without recurrence of symptoms. Patient 1 has followed up once five years after initial presentation with intermittent right sided abdominal pain approximately once or twice monthly, but she did not have any signs or symptoms of small bowel obstruction.
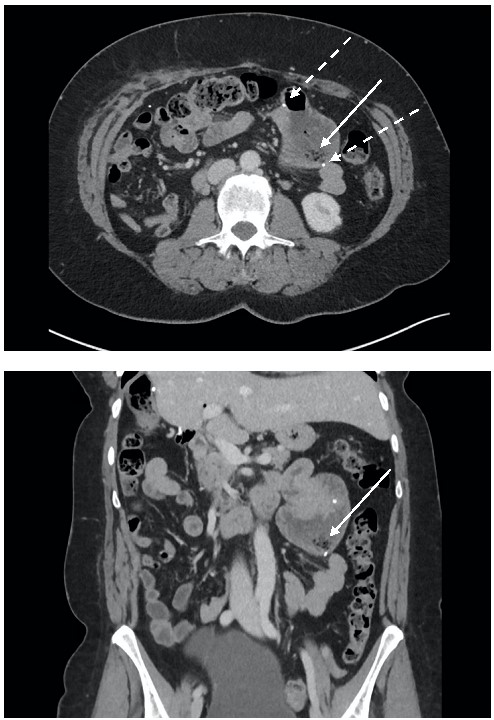
Figure 1: CT abdomen and pelvis with IV contrast with nonobstructing filling defect in the area of jejunojejunostomy. Filling defect shown with solid arrow. Note that the foci of air trapped in the bezoar are located dependently within the bowel lumen. Staple line shown with dashed arrows.
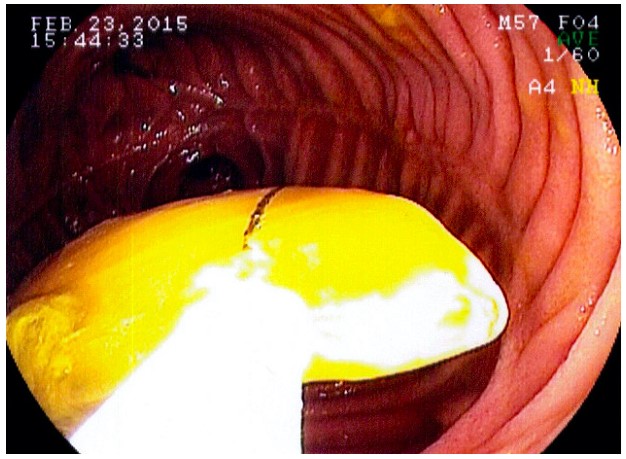
Figure 2: Endoscopic retrieval of bezoar with snare.
Case 2:
Patient number 2 is a 78-year-old female with a history of liver transplant in October 2011 for end stage liver disease secondary to non-alcoholic steatohepatitis. Her course was complicated by anastomotic common bile duct stricture, recurrent bile duct stones, and ascending cholangitis. She underwent multiple treatments with endoscopic retrograde cholangiopancreatography (ERCP) with stent placement. Her symptoms persisted, and she underwent Roux-en-Y hepaticojejunostomy in November 2018. This resolved her symptoms until approximately 4 months later in March 2019 when she presented with the first of multiple episodes of cholangitis. She was then maintained on alternating ciprofloxacin and Bactrim for prophylaxis. In January 2021, she presented to the emergency department with nausea, vomiting, and abdominal pain. Her medications at that time included: ursodiol, metoprolol, levothyroxine, levetiracetam, and famotidine. Initial lab evaluation showed hypochloremia (92 mEq/L), mild pancreatic enzyme elevation (lipase 178 U/L, amylase 177 U/L), mild leukocytosis at 12.5 K/MM3, direct bilirubin of 0.3 mg/dL, total bilirubin of 0.7 mg/dL, and normal transaminases (ALT 10 U/L, AST 18 U/L). CT abdomen/pelvis showed a small bowel obstruction with the transition point just distal to the jejunojejunostomy anastomosis. There appeared to be an intraluminal obstructing mass consistent with enterolith or bezoar. Push enteroscopy revealed a 3.5 x 2.5 cm stone impacted 15 cm past the jejunojejunal anastomosis and completely obstructing the small bowel lumen. The stone was fragmented using grasping forceps to create a core through the stone, and balloon dilation through the core was used to fracture the stone. The stone fragments were allowed to pass through the intestine. A nasogastric (NG) tube was placed for post-procedure decompression. On the following day, her abdominal pain was resolved, and CT abdomen/pelvis showed no remaining stone fragments in the small bowel with resolution of small bowel obstruction. Her NG output remained high at about 900 cc/day. The next day, a CT abdomen/pelvis with enteral contrast was performed, and the contrast passed into the colon. Her diet was advanced to general low fiber, and she was discharged uneventfully 4 days post enteroscopy. Since the admission for bowel obstruction, patient 2 has been readmitted once approximately 4 months later for recurrent cholangitis secondary to presumed intrahepatic duct stone formation, but she has had no recurrence of small bowel obstruction or abdominal pain.
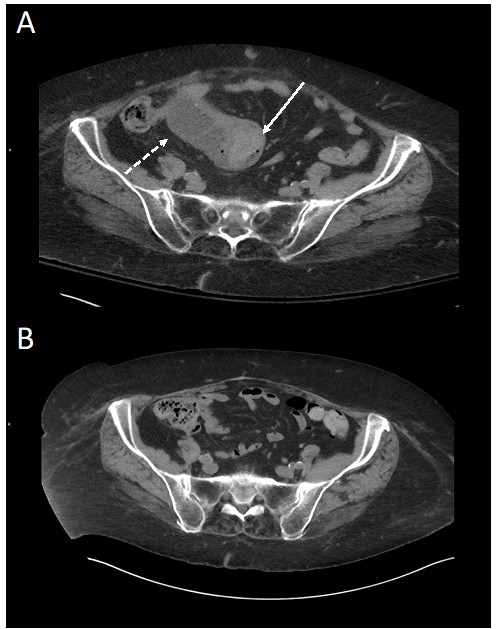
Figure 3: CT abdomen and pelvis with IV contrast with a solid intraluminal lesion in the area of the jejunojejunostomy. The solid lesion shown with solid arrow (A) is higher density than the fluid density components in the lumen shown with dashed arrow (A). Note the small foci of gas at the periphery of the lesion trapped within the interstices that are demonstrated on the subsequent endoscopy. Decompressed jejunum after endoscopic fragmentation of enterolith (B).
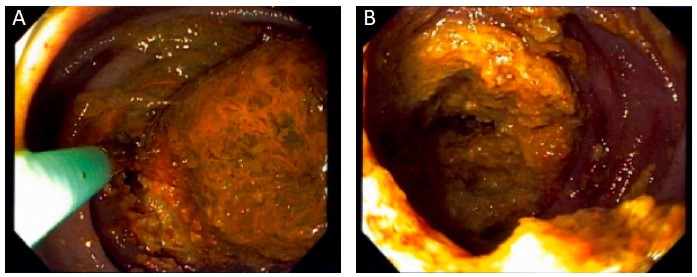
Figure 4: Endoscopic fragmentation of enterolith with endoscopic grasper (A). Center of the enterolith cored out prior to balloon fragmentation.
Case 3:
Patient number 3 is a 37-year-old female with a history of morbid obesity, chronic constipation, and hypertension who underwent an elective Roux-en-Y gastric bypass in 2015. She recovered well post-operatively, and she was discharged home on post-operative day 1 on a full liquid diet. Her diet was advanced to general bariatric diet. This consisted of eating three meals per day with 100 grams of protein and 100 grams of carbohydrates per day, drinking three 8 ounce servings of skim milk daily, avoiding fluids with meals, and drinking 6-8 cups of water each day. She was undergoing workup and treatment for chronic constipation which became worse after gastric bypass. This regimen included: daily use of miralax, biofeedback, unsuccessful trial of linaclotide, and fiber supplementation with 3.4 grams of Metamucil twice daily (started in November 2015). In June of 2016 she developed severe abdominal pain that was exacerbated by eating. She was initially evaluated in the Emergency Department with abdominal x-ray that showed no evidence of free air or obstructive gas pattern. It did demonstrate a large stool burden, and she was given multiple enemas which seemed to improve her symptoms, and she was discharged home. Her pain recurred 2 weeks later at which point a CT abdomen/pelvis was obtained and demonstrated a non-obstructing filling defect proximal to the jejunojejunostomy anastomosis. Esophagogastroduodenoscopy (EGD) was performed that day which demonstrated a large phytobezoar near the jejunojejunostomy anastomosis. This was mechanically broken up with a snare until the fragments were small enough to pass through the small intestine. This provided relief of her pain, and she was able to be discharged on the same day. She was instructed to avoid insoluble fiber in her diet, and she was given cellulase to take three times weekly. She did have subsequent development of intermittent abdominal pain in April of 2019, but EGD and CT abdomen/pelvis showed no abnormalities at that time.
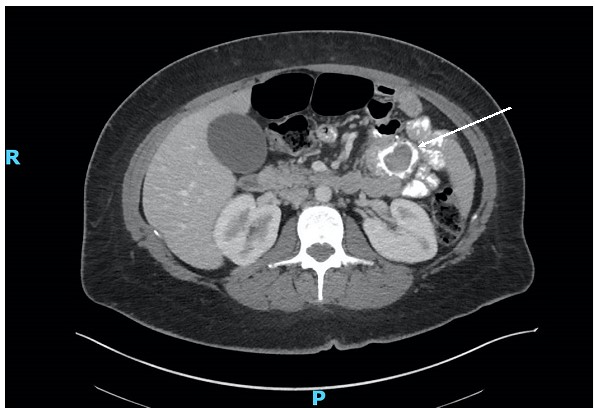
Figure 5: CT abdomen pelvis with IV and oral contrast with filling defect in the area of the jejunojejunostomy. Note that the filling defect shown with the solid arrow is outlined by the contrast on all sides and does not appear attached to the bowel wall.
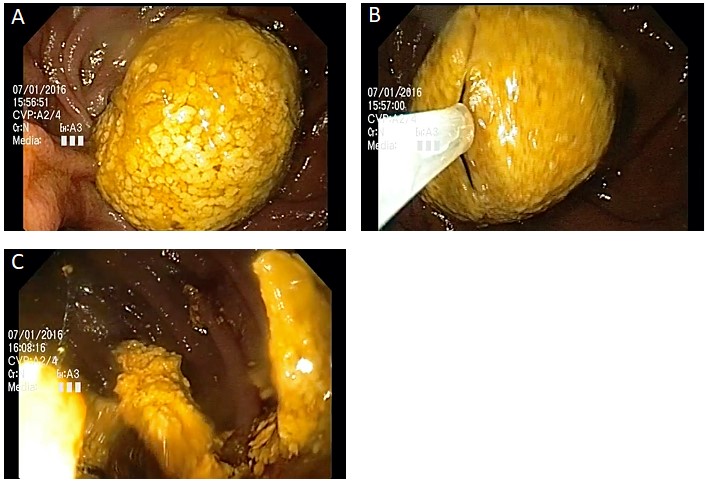
Figure 6: Endoscopic fragmentation of bezoar. (A). View of intermittently obstructing bezoar (B). Snare grasping bezoar (C). Bezoar pieces after snare fragmentation.
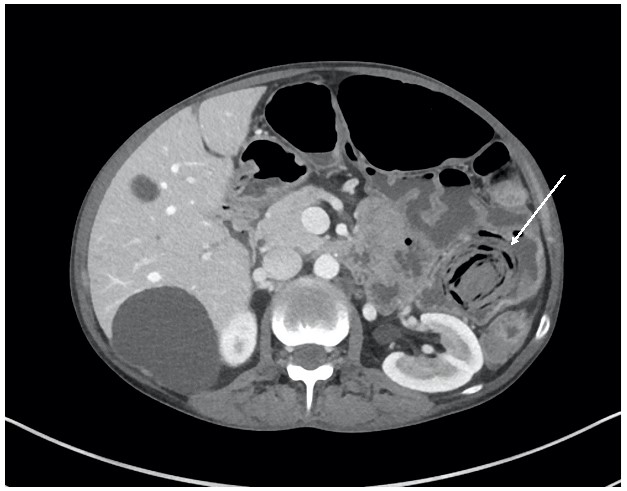
Figure 7: Classic appearance of bezoar in left upper quadrant dilated small bowel in patient with Crohn's disease. Note the layering curvilinear gas trapped within the bezoar.
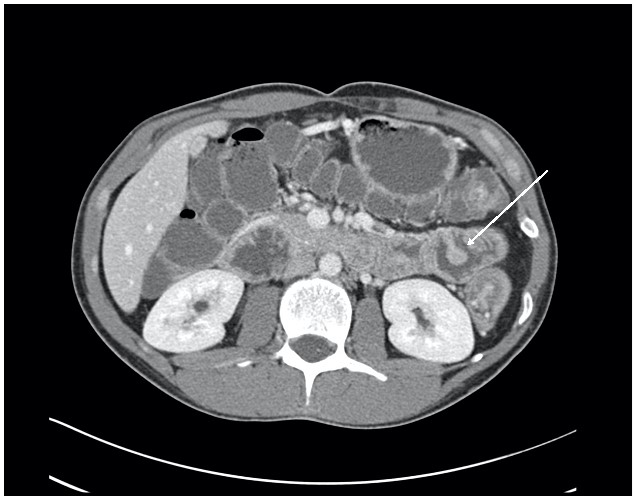
Figure 8: Classic appearance of jejunal polyp in patient with Peutz-Jeghers syndrome. Note the stalk attaching to the small bowel wall.
Discussion
Roux-en-Y reconstructions can be associated with a variety of complications, and these can generally be categorized into afferent and efferent limb problems. Afferent limb syndrome is when an obstruction occurs at or proximal to the jejuno-jejunostomy anastomosis leading to bile stasis, which can present with post-prandial epigastric pain that is relieved with vomiting. If the obstruction is high grade, ascending cholangitis can develop, particularly in the setting of a an upstream hepaticojejunostomy. Afferent limb syndrome is an uncommon complication, presenting in about 0.2% of cases following hepaticojejunostomy and in about 1.0% after Billroth II gastric bypass [7]. Efferent limb syndrome presents similarly to small bowel obstruction. The obstruction of either limb can occur due to post-surgical adhesions, internal herniation, or malignancy. Obstruction due to bezoar or enterolith is rare, but it has been reported. We present two cases in which patients developed small bowel obstruction from bezoar and enterolith formation after hepaticojejunostomy as well as a third case in which a bezoar was managed endoscopically in a patient with a Roux-en-Y gastric bypass.
Presentation
There are a small number of similar reports in the literature of enterolith formation following Roux-en-Y hepaticojejunostomy. The majority of these cases presented as cholangitis secondary to enterolith obstruction in the proximal afferent limb. Seven of the nine cases reviewed presented with proximal afferent limb obstruction with symptoms consistent with cholangitis: right upper quadrant pain, nausea, vomiting, and jaundice. Case 1 and 2 both presented with small bowel obstruction with enterolith/phytobezoar distal to the jejunojejunostomy. Whereas case 3 presented severe abdominal pain with a phytobezoar that was not completely obstructing the small bowel, but was thought to be intermittently obstructing with a ball valve mechanism. Case 1 showed no clinical signs or symptoms of cholangitis on presentation. The patient from case 2 had episodes of cholangitis both prior to and after the Roux-en-Y, but upon admission for small bowel obstruction had no signs or symptoms of cholangitis. Prior to the Roux-en-Y she was found to have a post liver transplant anastomotic stricture of the common bile duct which was treated with Endoscopic retrograde ERCP and balloon dilation. Subsequently this was also treated with stenting. After stent placement she continued to have episodes of cholangitis at which time ERCP showed multiple intrahepatic and extrahepatic stones which were cleared. Roux-en-Y was performed due to refractory episodes of cholangitis. At the time of operation a large stone was found in the common bile duct. The propensity for formation of multiple stones in the intra- and extrahepatic ducts seems to suggest that the obstructive stone likely originated from the bile duct system rather than forming in the small bowel primarily. The area that the stone obstructed was characterized by a 90 degree turn in the small bowel in a segment that was relatively fixed suggesting adhesions that may have predisposed this region to kinking. A stone that migrated from the bile duct system could have become lodged at this point due to mechanical kinking or hypomotility of the bowel and served as a nidus for further growth and eventual obstruction - akin to gastric outlet obstruction in Bouveret’s syndrome [8]. It is difficult to determine if the enterolith in case 2 ever contributed to her recurrent cholangitis, given the confounding prior history of intra- and extrahepatic biliary stones. However, the fact that her cholangitis was able to be managed successfully for about 2 years with prophylactic antibiotic treatment would argue against a complete obstruction of the afferent limb by the enterolith.
Mechanisms:
Contributing factors to stone formation include: bacterial overgrowth [9], dysmotility [10, 11], mechanical kinking of bowel [5, 12], foreign body nidus [13], and bile stasis [3]. An additional factor in enterolith formation in hepaticojejunostomy may be Roux limb length; two of the cases reported in the literature had afferent limb lengths of 70 cm which was thought to contribute to bile stasis and enterolith formation [10, 11]. Generally it has been recommended to make at least a 30 cm Roux length to prevent bacterial colonization of the bile duct; however, some groups advocate for a shorter Roux limb (20 cm) with the assertion that complication rates are similar and the success of endoscopic intervention in these shorter loops is higher [14]. Excess length of the Roux limb may contribute to dysmotility and bile stasis. Furthermore, Le Blanc-Louvry et al conducted a study using manometry which suggested that hepaticojejunostomy results in dysmotility in the Roux limb even in asymptomatic patients [15]. This baseline dysmotility coupled with excess length may increase the risk of bile stasis, bacterial overgrowth, and enterolith formation.
Medications are another potential factor in enterolith formation. Ursodiol (ursodeoxycholic acid) has been used to prevent recurrence of gallstones and common bile duct stones [16]. Ursodiol is a bile acid present in small amounts in human bile, and it is more hydrophilic than other bile acids [17]. This allows it to solubilize cholesterol stones and other bile acids [18]. However, Mukai et al reported an enterolith composed almost entirely of ursodeoxycholic acid in a patient who was receiving 600 mg ursodeoxycholic acid daily, suggesting that ursodiol supplementation could contribute to enterolith formation [6]. Quillen et al also reported a case of enterolith in a post liver transplant patient taking ursodeoxycholic acid. Interestingly, two of our patients were maintained on ursodeoxycholic acid before their presentations.
Radiologic Features:
Bezoar and enterolith have distinct radiologic characteristics. On CT, bezoars will generally appear as a dependent mass with a layered appearance of gas and solid components. Enterolith also appears as a layered dependent mass, however the mass does not contain gas. These can be distinguished from other endoluminal masses based on CT scan appearance. Lobulated intraluminal tumors will have an attachment to bowel wall [19]. Figure 8 shows classic imaging findings of jejunal polyp from a patient with Peutz-Jeghers syndrome. The mixed gas and solid components of the bezoar can appear similar to fecal material. It can be distinguished from fecal material by possessing a generally more discrete, ovoid shape, whereas, small bowel fecalization generally occupies a longer segment of bowel and is more amorphous [20]. Imaging in our study showed some classic and non-classic findings. Case 1 was determined to be a bezoar; CT scan findings supported this, showing a dependent ovoid mass containing solid and gas components (Figure 1). Case 2 had imaging characteristics consistent with enterolith. The mass appeared dependent, layered, and without air (Figure 3). Endoscopy confirmed these findings with impaction of a large, dense, hard enterolith that was difficult to fragment (Figure 4). Case 3 showed imaging characteristics more classic for enterolith. There is a dependent mass that appears layered, and there was no gas observed in the structure (Figure 5). However, endoscopy demonstrated a phytobezoar that was easily fragmented with an endoscopic snare (Figure 6). Figure 7 shows classic CT findings of bezoar. An oval shaped mass is seen in the dilated left upper quadrant small bowel with layers of solid components and gas trapped dependently within the mass. This image was from a patient with active Crohn’s disease treated at our institution and was included as a classic example of bezoar appearance on CT.
Interventions:
Surgical excision through enterotomy at the level of the mass has been the mainstay treatment of small bowel enteroliths and bezoars [3, 12, 21]. Endoscopic management of small bowel enteroliths has been attempted, but has often been reported as unsuccessful [3, 6, 22]. Factors attributed to non-successful endoscopic treatment include the inability to reach the enterolith or an inability to fragment the enterolith. Double balloon enteroscopy is a relatively new endoscopic technique that allows for evaluation of more distal segments of small bowel. Diagnosis of a distal bezoar (150 cm) by double balloon enteroscopy with subsequent surgical removal has been reported [23]. This included one report of attempted endoscopy with inability to reach the enterolith [6]. Successful endoscopic removal of small bowel enterolith has also been reported [24], however this was a case with normal anatomy of stomach, duodenum, and jejunum. Lee et al described decompression of the Roux limb with a percutaneous catheter followed by an attempt at stone fragmentation and retrieval with a metallic stone basket. Kim et al described successful cholangioscopic lithotripsy with subsequent flushing of stone fragments [9]. However these interventions were performed for afferent limb obstruction, and there have not been reports of efferent limb obstructions relieved endoscopically in patients with Roux-en-Y anatomy. Our cases demonstrated efferent limb obstruction at or distal to the jejunojejunostomy, and they were all managed endoscopically. Case 1 was managed with retrieval of fragments by metallic basket. In case 2, push enteroscopy revealed an approximately 90 degree angulation at which point the stone was impacted 15 cm distal to the anastomosis. The bowel distal to the impaction was also relatively fixed, suggesting possible distal adhesions that predisposed this region to kinking. Case 3 underwent mechanical fragmentation of the phytobezoar at the jejunojejunostomy site with a snare.
Conclusions:
Our cases highlight a unique presentation of enterolith and bezoar in the setting of jejunojejunostomy. Whereas the majority of previously reported enterolith cases presented as ascending cholangitis due to afferent loop obstruction, our cases presented with efferent small bowel obstruction. Cases 1 and 3 had obstruction at the jejunojejunostomy while case 2 demonstrated an efferent limb obstructing enterolith distal to the jejunojejunostomy. The management of our patients was also unique. While most other enteroliths required surgery, our cases highlight the safety and success of endoscopic intervention to relieve efferent limb obstruction in patients with Roux-en-Y anatomy. Each of the patients in our series had successful management of small bowel obstruction without recurrence. This sheds light on endoscopy as a new durable option for management of efferent limb small bowel bezoars and enteroliths in patients with Roux-en-Y anatomy. Avoiding surgery, particularly in patients with complex previous operations, is beneficial and therefore there should be early consideration of endoscopic management in patients presenting with Roux-en-Y limb obstructions due to enterolith and bezoar.
Declarations:
List of Abbreviations:
CT – Computed Tomography
EGD - Esophagogastroduodenoscopy
ERCP- Endoscopic retrograde cholangiopancreatography
GI – Gastrointestinal
NG - Nasogastric
Consent to Participate and Ethic Statement:
Written informed consent was obtained and all participants consented to submission for publication. The study was submitted to the University of Iowa Internal Review Board (IRB) and was deemed to not require full IRB approval to proceed.
Availability of data and materials – not applicable
Competing Interests: The authors do not have any competing interests to disclose.
Funding: not applicable
Author Contributions
Mitch Patrick – writing, editing, conception and design of the study.
Daniel Katz - writing, editing, conception and design of the study.
Frederick Johlin – writing, editing, analysis of cases.
Rami El Abiad – writing, editing, analysis of cases.
David Kuehn – writing, editing, analysis of images.
Acknowledgements – not applicable.